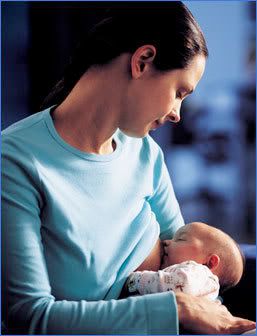
Happy Monday of World Milksharing Week!
This week is going to be all about the amazing stories of milksharing that we've witnessed and heard about through the different Human Milk 4 Human Babies communities over the past year. I've written several blogs about babies in need of breastmilk since starting Informed Parenting.
One of my favorite stories is about little Anaya in BC Canada, because her's is one that shows the power of community- even when it's not local. In the past year Anaya's mom Camara has received breastmilk donations from all over North America to feed her beautiful yet fragile daughter. http://iinformedparenting.blogspot.com/2010/10/breastmilk-for-anaya-in-nelson-bc.html
http://iinformedparenting.blogspot.com/2010/10/update-on-anaya-we-still-need.html
Another one of my favorite stories is about baby Jayden.
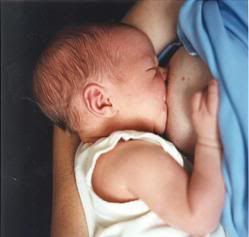
JAYDEN AT 10 WEEKS. BLIND AND DEAF.Jayden was born cocaine and alcohol addicted, with congenital syphilis, at 31 weeks gestation. She had no skin on the palms of her hands or feet and had to have skin grafts. They could find no formula that Jayden could tolerate well, but settled on the one that she had the "least severe reaction to."
When she was about eight weeks old, she was assigned a foster parent, who came to do kangaroo care with her for eight days before she took her home. Jayden was completely blind and profoundly deaf, and would need to be accustomed to "mom's" smell and touch before they sent her home. When she went home, she was the most critical discharge they have ever had from that NICU, which routinely sees the sickest of babies. Basically, with tears in their eyes, the nurses sent Jayden home to die. Jayden was insulin dependant (with critically unstable blood sugars, typically either below 60 or above 400), on oxygen 24 hours a day, and set off her apnea monitor 6-10 times a day. In order to set off a monitor, she would have to not breathe for many seconds at a time. She had gained and lost the same three ounces since birth, and was no more than four and a half pounds. Her foster mother asked over and over again of anybody who had authority why this baby couldn't be on breastmilk, shouldn't this baby be on breast milk, what did she have to do to get this baby on breastmilk? Over and over, she was basically told that this was a medicaid baby and that the state wouldn't PAY for banked milk (which costs a minimum of 4 dollars an ounce, and has been pasteurized) for a MEDICAID baby. Finally, one day, when Jayden was literally activly dying, an infectious disease doctor looked at her foster mom (who is a friend of mine because of foster work and doula work) and said, "I won't tell you NOT to give her breastmilk. We know that it would give her the best chance!" So, we got her some frozen breastmilk.
With her first bottle of human milk, Jayden's blood sugar regulated. She is typically somewhere around 120 now. Within the first three weeks, she regained her sight and hearing. Her new pediatrician says that when somebody is actively dying their brain will shut off all non-essential functions--and hearing and sight are non-essential functions. The first week on breastmilk she started to only set off her apnea monitor during the night's deepest sleep...and only then typically once a night. Within three weeks, they took it off of her completely, because she just didn't set it off any more. The first week she gained and KEPT ON four ounces. The next week three. The next week SEVEN. At this point, the new pediatrician put her arms around the Foster Mom's shoulders and said, "If you hadn't given that baby human milk when you did, she would be dead today. You are a hero." Eight weeks later she had gained nearly four pounds. When she was nearly nine and a half months old she was eleven and a half pounds! We now have full cooperation with her new pediatrician and the state to give her donated human milk, no questions asked.
With her first bottle of human milk, Jayden's blood sugar regulated. She is typically somewhere around 120 now. Within the first three weeks, she regained her sight and hearing. Her new pediatrician says that when somebody is actively dying their brain will shut off all non-essential functions--and hearing and sight are non-essential functions. The first week on breastmilk she started to only set off her apnea monitor during the night's deepest sleep...and only then typically once a night. Within three weeks, they took it off of her completely, because she just didn't set it off any more. The first week she gained and KEPT ON four ounces. The next week three. The next week SEVEN. At this point, the new pediatrician put her arms around the Foster Mom's shoulders and said, "If you hadn't given that baby human milk when you did, she would be dead today. You are a hero." Eight weeks later she had gained nearly four pounds. When she was nearly nine and a half months old she was eleven and a half pounds! We now have full cooperation with her new pediatrician and the state to give her donated human milk, no questions asked.
I also love the story of a good friend of mine Lynn, and her son Liam, Who struggled with supply issues. Lynn documented the changes in her little man, growing from a thin little waif to a chubby rollypolly happy baby after being fed breastmilk that had been donated by some wonderful women.
 Liam- two hours before being admitted to CHOP....
Liam- two hours before being admitted to CHOP...."Our pediatrician was uncomfortable with the EBM at first. She warned me about viruses and diseases and I told her I was more comfortable with the EBM then the Formula. I also told her we screened our donors. She asked me a few questions and smiled. She wanted to make sure we were being smart. And I would like to hope that todays mothers ARE being smart.
In June my son weighed 8 lbs.In September 14 lbsIn October 17 lbsAnd now (Dec 2010) weighs almost 20 lbs"